
Cancer risk and survival in Europe depending on where your cradle is located
Cancer is a major public health problem in Europe. In 2022, there were an estimated 2.78 million new cases of cancer in the 27 member states of the European Union (EU27) plus Iceland and Norway (EU+2 countries), equivalent to about five new diagnoses every minute. Cancer is expected to be the leading cause of death in Europe by 2035. The disparities in Europe are great and we need to address these disparities at the European level. That is the message of the newly released report Beating Cancer Inequalities in the EU: Spotlight on cancer prevention and early detection by the European Cancer Inequalities Registry (ECIR) and OECD (Organization for Economic Co-operation and Development).
There are many factors that determine your risk of cancer or of dying from it, including socioeconomic status (SES) and unhealthy lifestyle habits. But the country you live in also counts. Is there an effective national prevention policy with easy access to population screening and vaccination programs? How quickly are new cancer medicines available? All factors that contribute to a better chance of survival. Specifically on all these factors, the differences are significant within Europe.
In a European context, the Netherlands is praised for its cancer registry, rapid access to new cancer medicines and extensive population screening. But there are still areas where improvement is needed, such as reducing disparities between different socioeconomic groups. On Feb. 20, IKNL will release its own report on the relationship in the Netherlands between income groups and cancer incidence and stage at diagnosis.
Sharing best practices
To address these inequalities in cancer, the report calls for coordinated efforts at the European level. Through keen monitoring, both best practices and undesirable developments within Europe can be quickly identified and shared. To this end, it is crucial to sustainably fund European cancer registries, speed up the registration process in many countries, and break down barriers in (the interpretation of) privacy laws so that data from European countries can be linked and compared. In this way we can generate more new insights to reduce the impact of cancer in a targeted way.
How does the Netherlands actually score?
In some areas, the Netherlands is doing quite well, but we can also learn (enough) from other countries. The Netherlands was one of the last countries to have a national cancer plan. The Dutch Cancer Collective (initiated by IKNL, KWF and NFK) finally launched the National Cancer Agenda in November 2023. This plan contributes to the Netherlands' efforts within the European Beating Cancer Plan. This contains five prioritized goals: smoking behavior, early detection, rare cancers, (late) consequences, and work and cancer.
Cancer death rates are up to 1.6 times higher in some countries
While the number of cancer diagnoses increased between 2010 and 2022 in 14 of the 24 countries with available data, cancer deaths in the EU27 declined by 10% over this period, with declines seen for most cancer types. However, cancer mortality remains high (22.5% of all deaths) and is up to 1.6 times higher in some EU+2 countries than in others. For many cancers, higher mortality rates are found in Central and Eastern European countries (Croatia, Hungary, Latvia, Slovakia and Slovenia), while Western and Northern European countries (Finland, Luxembourg, Spain and Sweden) have the lowest mortality rates. The Netherlands is in the middle range.
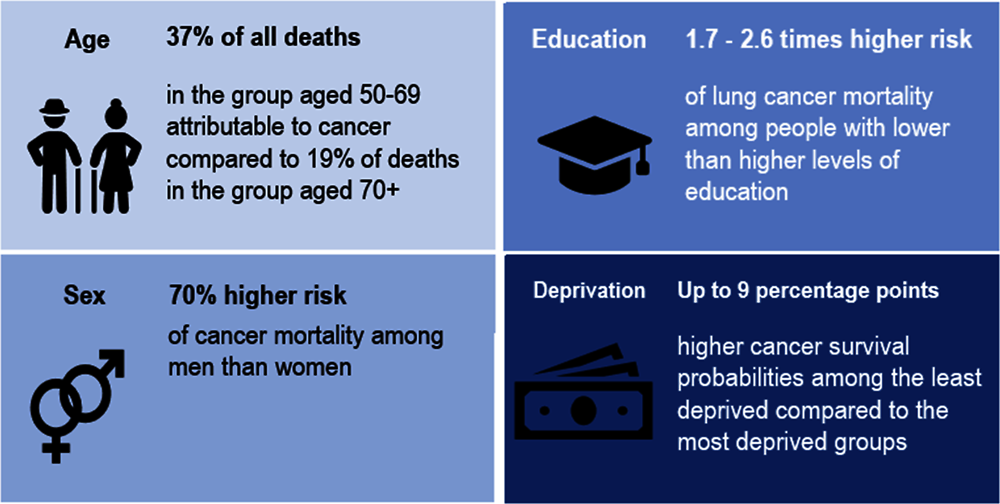
Not everyone has the same risk of dying from cancer, even in different regions within the same country. Cancer mortality rates differ up to 37% between regions in Romania and at least 30% between regions in France, Germany, Poland and Spain. Men have almost 70% higher mortality rates than women. Moreover, men with lower levels of education are 2.6 times more likely to die from lung cancer than men with higher levels of education; for women, 1.7 times more.
 Unhealthy lifestyle, metabolic risks and poor environment explain more than 40% of cancer burden
Unhealthy lifestyle, metabolic risks and poor environment explain more than 40% of cancer burden
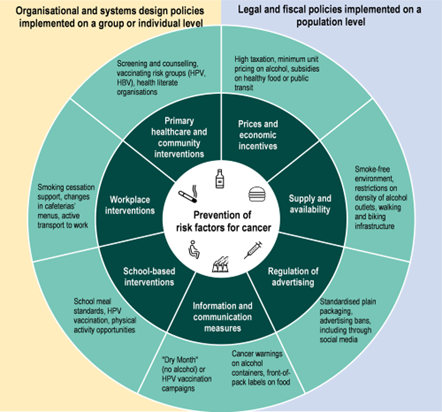
By far the most important risk factor for cancer mortality in EU+2 countries is tobacco (more than a quarter of cancer deaths are attributed to smoking), followed by alcohol consumption, unhealthy diet, occupational hazards, overweight and obesity, high blood sugar, air pollution, physical inactivity and infection with three types of viruses: human papillomavirus (HPV) the hepatitis B virus and hepatitis C virus. The main risk factors for cancer are more common in Europe among people with lower socioeconomic characteristics. There are also large differences in cancer risk factors by gender at the expense of men - particularly for smoking, alcohol consumption, poor diet, overweight and obesity. In EU27 countries, men are 51% more likely to smoke daily than women and alcohol consumption is twice as common compared to women.
Comprehensive prevention policies targeting vulnerable populations
Since we can prevent 40% of cancer deaths, we need to put much more effort and money into effective prevention policies, at national and European level. Most member states, according to the report, invest too little in prevention: by 2021, an average of only 5.1% of total health spending in the EU27 will be spent on prevention. To counter alarming trends in cancer incidence and inequality, fundamental prevention policies are needed to address cancer risk factors, targeting high-risk populations. Disparities to the detriment of low SES groups in participation in cancer screening and vaccination programs must also be addressed by devising ways to better reach vulnerable populations.
Screening alone is insufficient for early detection; it starts with awareness
Screening for breast, cervical and colorectal cancer increases the chances of early detection and thus improved survival. Despite the fact that most EU countries have screening programs for breast, colorectal and cervical cancer, participation rates vary widely and are worryingly low in many countries. In 11 EU+2 countries, less than half of women aged 50-69 have had a mammogram in the past two years. This report shows that in countries with higher participation in breast cancer screening, breast cancer survival is better. There are also differences in cancer screening rates to the detriment of groups with lower education or income levels: the percentage of women with low SES who have had a mammogram is 15% lower. In addition, people with low SES are less likely to get vaccinated than those with high SES.
Achieving higher attendance in cancer screening and vaccination programs begins with increasing cancer awareness, especially among vulnerable populations. This includes increasing knowledge about the symptoms of cancer and the benefits of participating in population screenings, in which general practitioners play an important role. But also developing education programs for those with low literacy and limited health literacy.
Conclusion
Overall, this report shows that much remains to be done in Europe to address the increasing burden of cancer and inequalities therein.
- by investing in comprehensive prevention policies with a special focus on vulnerable groups
- ensuring widely accessible screening
- high vaccination coverage
- rapid availability of new medicines
- and comparing cancer burden between European countries and selecting best practices.
About this report
This report is based on the Country Profiles on Cancer of EU countries and the European Cancer Inequalities Registry, (ECIR). It examines policies and actions to reduce the impact of cancer, with a focus on addressing preventable risk factors and improving the reach of screening and early diagnosis to counter alarming cancer trends and inequalities.
The European Cancer Inequalities Registry (ECIR) is an initiative of the European Beating Cancer Plan. It provides reliable data on cancer prevention and care to identify trends, inequalities and disparities between member states and regions.
ECIR has now delivered 3 milestones:
- ECIR data tool (2022). This tool provides an interactive way to compare indicators of inequalities in cancer prevention and care across Europe.
- Publication of 29 country profiles on cancer (2023). Country profile for the Netherlands 2023
- Report "Beating Cancer Inequalities in the EU: Special focus on cancer prevention and detection" (2024).
IKNL's role in development of this report
All European countries participate in the working group around the European Cancer Inequalities Registry and make agreements around research and further development of ECIR. IKNL participates with extensive data and interpretation from the Netherlands Cancer Registry (NCR) on behalf of the Netherlands. Insights from ECIR are translated into the National Cancer Agenda through the Dutch Cancer Collective.
More information
Gijs Geleijnse, management consultant on innovation and internationalization and member of the steering committee of the European Network of Cancer Registries (ENCR)
Jelle Evers, junior clinical data scientist